Learninsta presents the core concepts of Microbiology with high-quality research papers and topical review articles.
Overview of an Transplantation
Transfer of living cells, tissues or organs from one part of the body to another or from one individual to another is known as transplantation. A tissue or organ that is removed from one site and placed to another site usually in a same or different individual is called graft. The individual who provides the graft is called donor and the individual who receives the graft is called host or recipient.
If the graft is placed into its normal anatomic location, the procedure is called orthotopic transplantation. If the graft is placed in a different site it is called heterotopic transplantation. Transplantation is the only form of treatment for most end-stage organ failure.
In clinical practice, transplantation is used to overcome a functional and anatomic deficit in the recipient. Transplantation of kidneys, hearts, livers, lungs, pancreas and bone marrow are widely done today.
Methods of Transplantation
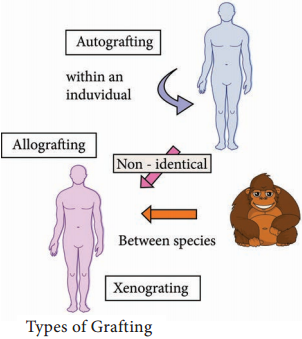
Auto grafting:
The transfer of self tissue from one body site to another in the same individual
Allografting:
The transfer of organs or tissues from human to human
Xenografting:
The transfer of tissue from one species to another (Figure 11.11).
Graft Acceptance
When transplantation is made between genetically identical individuals the graft survives and lives as healthy as it is in the original places. When the graft tissue remains alive, it is said to be accepted and the process is called graft acceptance.
Graft Rejection
When transplantation is made between genetically distinct individual the graft tissue dies and decays. When the graft tissue dies, the graft is said to be rejected and the process is called graft rejection. It is of two types. They are:-
- Host Verses Graft Reaction
- Graft Verses Host Rejection.
Host Verses Graft Reaction (HVG)
The graft tissue antigens induce an immune response in the host. This type of immune response is called host versus graft reaction.
Allograft Rejection
Types of allograft rejection
- Acute rejection-Quick graft rejection. It is due to stimulation of thymocytes and B lymphocytes
- Hyperacute rejection-It is a very quick rejection. It is due to pre-existing humoral antibodies in the serum of the host as a result of presensitization with previous grafts.
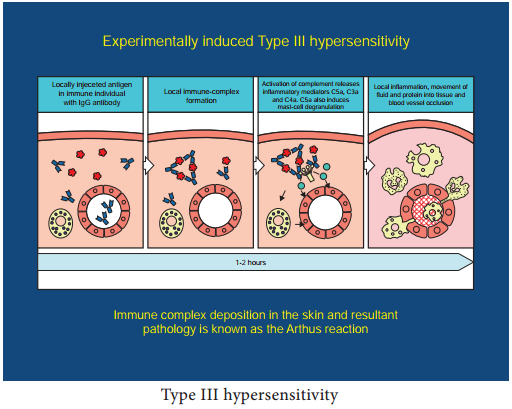
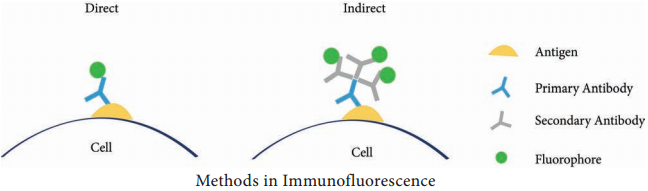
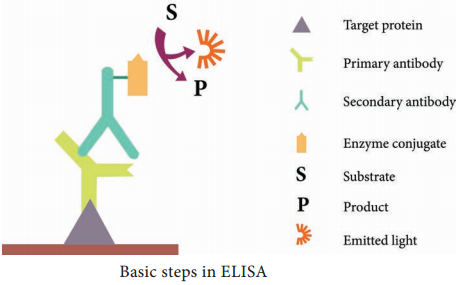
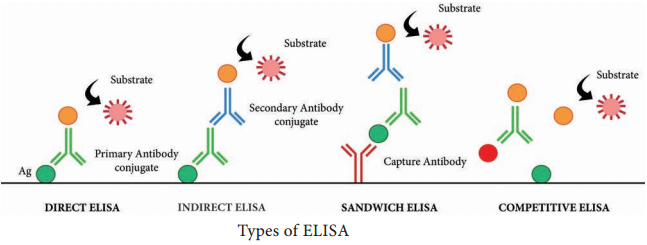
- Insidious rejection-It is a secret rejection due to deposition of immune complex on the tissues like glomerulus membrane that can be demonstrated in kidney by immune fluorescence.
Mechanism of Allograft Rejection
Immunological contact
When tissue is implanted as graft, its antigen can pass into local lymph nodes of the host. The graft antigens then make contact with the lymphocytes of the host. Production of sensitized T cells and cytotoxic antibodies are produced in the host. This brings about graft rejection.
First set rejection
When the graft is made between genetically different individuals, the graft gets blood supply from the host and it appears to be normal for the first 3 days. But on the 5th day, sensitized T cells, macrophages and a few plasma cells invade the graft. Inflammation starts in the graft. This leads to necrosis. It is similar to the primary immune response to an antigen.
Second set rejection
When a graft is implanted in an individual who has already rejected a graft is second set rejection. This is similar to the secondary immune response of our body.
Cell mediated cytotoxic reaction
The 1st set of rejection of allograft is brought about mainly by CMI response. In this process the cells involved in the cytotoxic mediated immunity involves. On stimulation of these cells interferon causes the lysis of the graft.
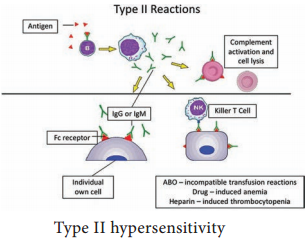
Antibody mediated cytotoxic reaction
The 22nd set rejection of graft is brought about mainly by HMI response. This is one of the hyperacute rejection brought about by the antibodies. Complement, macrophages, mast cells, platelets, B cells bring about this reaction.
Graft versus Host Rejection (GVH)
Sometimes the graft tissue elicits an immune response against the host antigens. This immune response is called graft versus host reaction. It occurs when:
- Graft remains inside the host and the host should not reject the graft.
- The graft should have immune competent T cells.
- The transplantation antigens of the host should be different from that of the graft.
Mechanism of the graft rejection
The graft lymphocytes aggregate in the host lymphoid organs and are stimulated by the lymphocytes of the host. The stimulated lymphocytes produce lymphokines. Lymphocytes in turn activate the host T cell. Activated T cell further activates the B cells. The stimulated B cell reacts with the self antigen and causes the damage.
How to prevent graft rejection?
Before transplantation the following things should be done to avoid graft rejection.
- Perform blood grouping and Rh grouping
- HLA typing should be done
- Immuno suppressive drugs should be administered
- Suitable donor should be chosen